Origins of Cognitive-Behavioral Therapy
The evolution of Cognitive-Behavioral Therapy (CBT) stems from the integration of behaviorism and cognitive psychology. Initially, behaviorism, emerging in the early 20th century, focused solely on observable behaviors, emphasizing that all behavior is learned through conditioning and can be modified using reinforcement or punishment. This approach was practical and structured but neglected the role of internal thoughts and emotions.
In the 1960s, cognitive theory, pioneered by psychologists like Aaron Beck and Albert Ellis, introduced the idea that thoughts significantly influence emotions and behaviors. This marked a shift toward understanding the internal mental processes that contribute to psychological distress, such as irrational beliefs or negative thought patterns. Cognitive therapy aimed to help individuals identify and challenge maladaptive thoughts to create positive changes in emotions and actions.
Modern CBT merges these approaches, combining the structured, evidence-based techniques of behaviorism with the emphasis on cognitive restructuring from cognitive psychology. Today, CBT is a holistic, flexible model that addresses both thought patterns and behavioral changes, incorporating insights from neuroscience, mindfulness, and emotion regulation for a comprehensive approach to mental health. This evolution has made CBT one of the most effective and widely-used therapeutic methods worldwide.
Core Principles of Cognitive-Behavioral Therapy
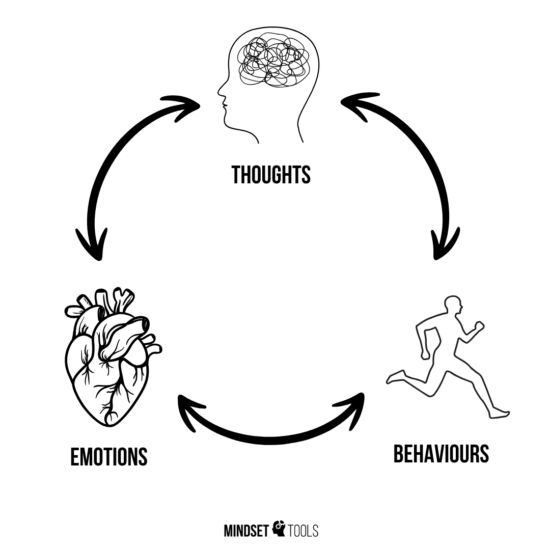
The Cognitive Model: Thoughts, feelings, and behaviors are interconnected, and distorted or maladaptive thinking patterns can lead to emotional distress and unhealthy behaviors. Changing negative thought patterns can improve emotions and actions.
Goal-Oriented and Problem-Focused: CBT addresses specific issues through collaboratively set goals, providing a clear focus for therapy sessions.
- Based on a Continuously Evolving Case Conceptualization: CBT relies on an ongoing assessment and conceptualization of the patient’s problems and functioning in cognitive terms to guide the therapeutic process effectively.
Structured and Time-Limited: Therapy is organized and typically short-term, lasting between 6 to 20 sessions, with a focus on education, skill-building, and practice. The exception is therapy for personality disorders, which may require long-term work, or cases involving multiple co-occurring disorders. However, it is the patient who decides what they would like to focus on and what would serve as a measure of problem resolution.
Active Collaboration: The therapist and client work as a team, fostering a collaborative and empowering relationship where clients take an active role in their progress.
Identifying and Changing Cognitive Distortions: Clients learn to recognize and challenge cognitive distortions like catastrophizing, black-and-white thinking, and overgeneralization, developing healthier, more balanced thoughts.
Behavioral Interventions: Techniques such as exposure therapy, behavioral activation, and skill-building exercises are used to confront fears, build confidence, and establish positive habits.
Skill Development and Relapse Prevention: CBT focuses on equipping clients with practical tools like mindfulness, emotional regulation, and problem-solving to handle future challenges and maintain progress.
Evidence-Based Approach: CBT is grounded in scientific research and consistently updated to ensure its effectiveness across a wide range of mental health conditions.
By integrating these principles, CBT provides a structured, practical framework for achieving lasting emotional and behavioral change.
Evidence based treatment
CBT is one of the most extensively researched and evidence-based forms of psychotherapy, consistently demonstrating high efficacy in treating a range of mental health conditions, including anxiety, depression, PTSD, and OCD. Its structured, goal-oriented approach is supported by rigorous scientific studies. For example, the NICE (National Institute for Health and Care Excellence) guidelines in the UK frequently recommend CBT as the first-line treatment for many mental health disorders, emphasizing its proven effectiveness and safety. This endorsement reflects CBT’s science-based approach, making it a trusted choice for both clinicians and patients worldwide. Additionally, CBT provides evidence-based strategies to address issues that are not limited to specific diagnoses, including difficulties like low self-esteem, managing anger, procrastination, perfectionism, and other personal challenges.
Is online therapy effective?
Online therapy has emerged as an effective alternative to traditional in-person sessions, particularly in treating conditions like anxiety and depression. A study published in the Journal of Medical Internet Research found that internet-based cognitive behavioral therapy (iCBT) is as effective as face-to-face therapy for these disorders, offering comparable outcomes in symptom reduction and patient satisfaction (PLOS Journals). Additionally, the American Psychological Association reports that both patients and providers view telepsychology favorably, noting its effectiveness and the convenience it offers (American Psychological Association). These findings underscore the viability of online therapy as a credible and accessible option for mental health care.